How frequent do you encounter lying patients at your work?
According to a 2015 US survey, 46% of Americans avoided telling health issues to their medical providers because of embarrassment. This is not surprising to know as most patients are ashamed of their health problems and don’t want to be scolded for their poor lifestyle. Unfortunately, patients fail to take into consideration that providing their doctors and nurses with accurate information is crucial in getting them the proper medical attention they need for their care.
If you are feeling naïve in detecting a lying patient, take a look at the following top ten lies patients say to their nurses. Are you familiar with any of these?
1“I rarely smoke.”

Smoking is an addictive habit because of nicotine. It’s hard to abruptly stop cigarette smoking without professional help. When your patient tells you that he rarely smokes or he already stopped smoking several months ago, let the patient elaborate. By elaborating, you can determine your patient’s definition of stopping or limited use.
Tip: If your patient tells you that he rarely smokes, let him estimate the number of cigarette sticks he consumes per week. But if your patient claims total smoking cessation, look for physical signs. Smokers’ breath smell like cigarettes even hours after they last smoked. You can also notice distinctive yellowing of teeth and darkening of gums among chronic smokers.
Also, ask your patient about usage of e-cigarettes or vapes. Most people don’t consider using these devices equal with cigarette smoking.
2“I drink occasionally.”
When asked about drinking habits, patients typically answer “occasionally”. By digging deeper, you will be surprised to know that their occasional drinking is actually a consistent habit. The amount of alcoholic drink consumed is also tricky to ask. They usually say “a few glasses” without revealing the exact number of glasses consumed or how large their glass is.
Tip: Be objective in determining your patient’s alcoholic drink consumption. Ask about how often per week the patient drinks. Also, let the patient estimate the volume of alcoholic beverages he consumes by mL or liters.
3“I’m physically active.”
When assessing physical activity, some patients are quick and defensive to say that they have a very active lifestyle. They are proud to say that they frequently go to the gym or jog around the park when in fact, they just do it once or twice a month. Most patients tell lies about their physical activity to elicit good impressions on their lifestyle habit.
Tip: Whenever you suspect lying patients when doing assessments about physical activity, ask about the frequency of their exercise regimen. If they say that they exercise regularly, look at their body build as it should be evident in their physique.
4“I follow the recommended diet for me.”
A lot of patients are guilty of bad eating habits. When prescribed with a particular diet, it’s hard to follow the changes at first so some patients just lie and don’t admit their eating splurges. Their weight, laboratory works and vital signs can tell the truth so it’s easy to know if the patient is lying about his diet.
Tip: If you suspect that your patient is lying about his eating habits, discuss the importance of adhering to the prescribed diet. Talk about how poor diet can affect his health and how it can prompt changes in his treatment plan. The idea of having more diagnostic examinations and taking more medications is usually enough for the patient to take his diet seriously.
5“I always take the medications prescribed to me.”
This is a common lie among patients with chronic health problems like diabetes and hypertension. They will claim that they don’t skip taking the prescribed medications to them when in fact, they don’t take their pills whenever they feel asymptomatic. This is also a usual problem among patients taking herbal supplements as they think natural remedies can adequately replace their maintenance medications.
Tip: If you are suspecting that your patient is lying as his laboratory works don’t reflect adherence to prescribed medications, ask about any side effects felt when taking the prescribed pills. You should expect to hear the likely side effects of the drugs prescribed. But if you hear unusual and more serious side effects from the patient, ask if encountering them made him skip taking the prescribed medications. Stress the importance of telling the truth so his doctor can modify his medications to more efficient ones
6“I only take medicines prescribed by my doctor.”

Most patients don’t want to admit self-medication. It’s either because they feel embarrassed or they don’t want to be admonished as they know that it’s wrong. They usually self-medicate with pain relievers, anti-histamines, antacids and laxatives. Not admitting how they self-medicate is dangerous as it can produce adverse drug reactions when taken with other prescribed medicines.
Tip: When asking about use of non-prescribed medications, cite examples to the patient. Mentioning paracetamol, mefenamic acid, bisacodyl and other over-the-counter drugs will ring a bell in their memory. Stress the importance of listing over-the-counter drugs taken in ensuring safe treatment plan. Also, ask about herbal supplements and vitamins taken as they can produce adverse drug reactions when taken with other medications. .
See Also: 5 Tips On How to Manage Patients Who Self-Diagnose
7“I don’t have sexual problems.”
Discussing sexual habits, including sexuality and number of sexual partners, is uncomfortable for everyone. However, this is a normal thing to discuss among healthcare providers as it is routinely included in total physical assessment of adult patients.
Patients should be informed why it’s important to get an accurate assessment of their sexual activity so they will be honest with themselves. Sexual problems can be part of the symptoms for an undetected medical condition. Risky sexual behavior can also indicate the need for further examinations. For example, poor libido or erectile dysfunction may indicate underlying medical problem while poor sexual habits may indicate need for further laboratory examinations to test for Sexually Transmitted Infections (STIs).
Tip: Discussing sexual history is a sensitive topic for patients. Before doing this, make sure to establish good rapport. Talk first about why you need to do this assessment and why it is important for the patient’s health.
8“My symptoms first started when…”
For healthcare providers, knowing when the symptoms first started is important to determine acute or chronic underlying diseases. This detail is often taken for granted by most patients. Instead of giving a well-thought estimated range of dates for the onset of their symptoms, they are quick to claim a random timeframe. This can be dangerous especially if an undetected underlying problem is a time-ticking bomb like an aneurysm or an aggressive form of cancer.
Tip: If the patient can’t remember when his symptoms first started, mention important occasions that may serve as a guide to know the exact onset of symptoms. Educate the patient about how important to know when the symptoms first started as acute problems need to be addressed quickly to avoid their progression to life-threatening conditions.
9“I don’t have any family history of that disease.”
Admitting family history of a particular disease is sometimes embarrassing for patients. Family history of mental health problems, cancer and other illnesses are just some of the information most patients keep from their healthcare providers due to fear of social stigma. This could be a hindrance to proper diagnosis and doctors may miss detecting a potentially dangerous health problem at its early stage.
Tip: Establishing good rapport is essential in getting accurate family history of illnesses. Be therapeutic in communicating to the patient and be careful with your non-verbal gestures when responding to their statements.
10“I always feel this bad.”
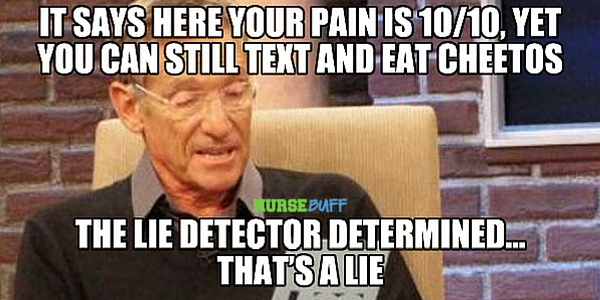
We all have different levels of tolerance for pain and other symptoms. However, there are patients who often exaggerate symptoms to get sympathy. Some patients are also doing it to get the pain relievers they were addicted with. Be careful when assessing these kinds of patients as it can be tricky to know if they are telling the truth or not.
Tip: For patients with exaggerated reports of symptoms, other means of doing assessment will be useful. Correlate diagnostic workup results and vital signs with the reported health problem. Use your clinical eye and pain rating scale. Associate the reported symptoms with the patient’s non-verbal cues. If the patient says 10/10 pain rating scale but can still smile while saying it, be suspicious and reassess after a few minutes.
See Also: Nurse Skills: How To Detect A Lie
Encountering lying patients at work is nothing new to nurses. Still, you should always encourage your patient to be honest to their healthcare providers. Let them understand that this is important in ensuring quality medical care for their health problems.




















