I remember the exact moment where I realized I was utterly and completely burnt out from nursing. At two o’clock in the morning on that night shift, it was a very, very close call that I didn’t quit the profession altogether.
It had started out as a long and busy shift, with admission after admission. Some of the cases very complex and there were acutely ill patients. Not to mention, we were short-staffed. The first set of nurses were finally leaving for a break. I took a report from my exhausted co-worker and sent her to the staff room, eager for my turn when she returned.
There was a merciful lull in the call bells and alarms. I was able to get caught up in most of my work. I stretched and left the nursing station to check in on the fourteen patients currently under my supervision.

Then, I noticed one of my partner’s patients- a frail, elderly gentleman– was banging incessantly on his bed railings. He had been doing these motions earlier in the shift and I had seen it when I rushed past the room.
At the time, swamped with my own assignment of patients, I had only been able to notify his nurse and leave it in her hands. It was looking like she had not had the time to investigate the behavior. I looked more closely at the information sheet she had given me before leaving on a break and my heart sank. The patient was an 86-year old gentleman who was deaf, mute, and blind.
I approached the bed and reached for his hand. His face changed immediately, clearly relieved to have finally captured someone’s attention. But his tight grip around my fingers showed an undertone of urgency. It was clear he was desperate to find a way to communicate what he needed.
Did he want to use to the bathroom? I had him feel the handle of the urinal. A shake of the head. Was he thirsty or hungry? I tried giving him a cup of water. A sandwich, a warm blanket, repositioning of his body… nothing seemed to help him settle. If anything, he seemed to be getting more panicked that I would give up or be pulled away before finding the root problem.
That’s when I saw it– a pattern in his motions.
Between the sign language that I was lost to interpret, I noticed a rub of his hand on his jaw. It finally clicked he did not know it was the middle of the night.
How could he? And he was asking for a shave.
I squeezed his hand repeatedly and patted his shoulder, excitedly hoping to communicate I finally understood. I put all my other tasks on hold that I could safely delay and came back with the supplies. The instant I placed some hot wet towels on his face, his face broke out into the happiest expression I had ever seen.

He started to cry and kept taking my hand and kissing it in thanks. That’s when I started crying myself. Full-on, uncontrollable sobs at two in the morning as I gave this gentleman a shave in the dark.
What kind of profession was I in where this man lay alone, unattended, and in anxiety for so many hours over something so simple?
My nursing license and my conscience hold me responsible to providing dignified and compassionate care. And yet shift after shift, I am not able, in any way, to meet these standards. I’m stuck working under a health care system that stretches nurses so thin where we barely have time to provide safe care, let alone hold the hand of someone who is scared, turn patients to prevent them from developing bed sores, help patients to the toilet when they need it or give a simple shave to a distressed man who is deaf, mute, and blind.
I was bitter. I was sad. And I had had enough. It was time to change careers.
This is not an isolated incident – nursing shortages are rampant nationwide. As much as we continue to fight for safe staffing levels in our workplaces, it is an uphill fight with no forthcoming solutions. We lose many nurses, especially new graduates, who are unable to cope with the burden of not being able to provide ethical and just care.
So, how do we help the nurses in immediate need of tools to cope with the moral distress of the profession? How do we keep them from quitting and placing further strain on an already strained system?
After my meltdown and some time off, I realized I didn’t want to quit- at least not yet. I am a good nurse- I’m proud of that- and my team would struggle to lose me. But I needed help. I was clearly burnt out.
I couldn’t ignore any longer the stress of not having enough resources to provide the care that I valued, combined with the daily witnessing of human suffering and the rampant violence that plagues the profession.
The Surprising Answer
So, I turned to the internet to find some tips on how to avoid burnout in healthcare. What are the recommended strategies for mitigating risks of burnout? Keeping a journal, practicing self-care, maintaining a work-life balance, reducing work stress, learning self-awareness strategies, maintaining relationships- they sounded great on paper. However, in practice, I found the ideas to be too broad, time-consuming or unrealistic.
Yet something that piqued my interest during my research was the concept of “positive psychological interventions”, specifically gratitude therapy. Just saying “thank you”. Simple, attainable- something I could start the very next day at work.

The research was cohesive: expressing gratitude freely and frequently had the potential to enhance personal and professional wellness and resiliency, as well as workplace culture and teamwork.
I resolved to go back to work but prepared by carrying around some “gratitude cards” in my scrubs. They were short, pre-written thank-you messages that I could easily and quickly share with a co-worker no matter how busy the shift.
As I started handing them out, I saw an immediate positive response from my co-workers. The teamwork was more positive and there was a lighter mood on the unit. Patient care improved because our team relationships improved. Not only that, but there was lightness within myself.
With my gratitude cards in my pockets, tucked in between my stethoscopes and many pens, I felt happier and more prepared to face the stresses of nursing.
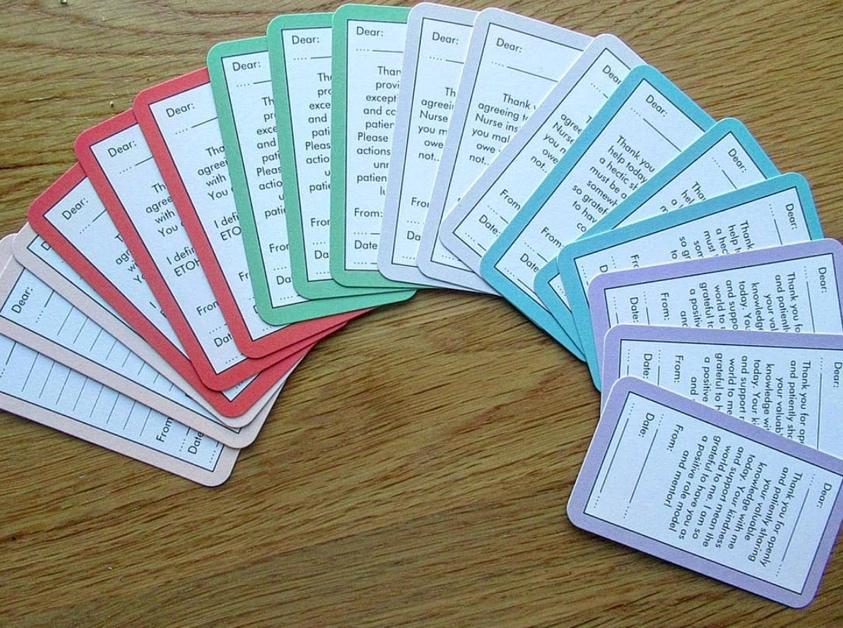
Gratitude cards have helped me come back from the lowest point in my career, where I found myself crying in between dark curtains giving a patient a shave. In the spirit of sharing coping strategies with my fellow nursing community, I highly recommend trying out some self-made cards or purchasing pre-made ones, such as are available on littlethanks.ca, as a quick and easy way to reap benefits of sharing gratitude frequently and freely.
What strategies have you found helpful in your workplace to promote physical and psychological resiliency? What are your experiences with burnout and compassion fatigue?
See Also: Mind Healing: DIY Gratitude Journal Ideas
 Isabelle is a Registered Nurse and Quality Improvement Clinician at a busy Canadian urban hospital. She is also the founder and creator of Littlethanks Cards for Nurses, which can be purchased at littlethanks.ca.
Isabelle is a Registered Nurse and Quality Improvement Clinician at a busy Canadian urban hospital. She is also the founder and creator of Littlethanks Cards for Nurses, which can be purchased at littlethanks.ca.


















