Getting familiar with and interpreting laboratory values can be intimidating, particularly to new nurses. There’s always the fear of messing things up and not being able to meet the patients’ health needs.
But, guess what?
Familiarizing and interpreting laboratory values for nurses don’t always have to feel that way. With the right tips, you’ll be able to overcome those fears and complete your tasks easily.
Let’s get started.
Also Read: Nursing Mnemonics and Tricks for Nurses (Diagnostics)
![]()
I. Complete Blood Count
![]()
Complete blood count is one of the most basic laboratory examinations to assess the overall health status of a patient. It can help diagnose infections, autoimmune disorders, anemia, and other blood diseases.
A. Red Blood Cell (RBC)
The red blood cells’ primary function is to carry oxygen from the lungs towards your body tissues and carry carbon dioxide away from those body tissues to the lungs.
Normal range:
Male: 4.5–5.5 x 1012/L
Female: 4.0–5.0 x 1012/L
Children: 3.8–6.0 x 1012/L
Newborn: 4.1–6.1 x 1012/L
High Level: Dehydration, cigarette smoking, congenital heart disease, pulmonary fibrosis, renal cell carcinoma, polycythemia vera
Low Level: Bleeding, anemia, malnutrition, overhydration, hemolysis, erythropoietin deficiency, leukemia, multiple myeloma, porphyria, thalassemia, sickle cell anemia
Drugs that may increase RBC count: Methyldopa, gentamycin
Drugs that may decrease RBC count: Quinidine, hydantoins, chloramphenicol, chemotherapeutic drugs
B. Hemoglobin (Hgb)
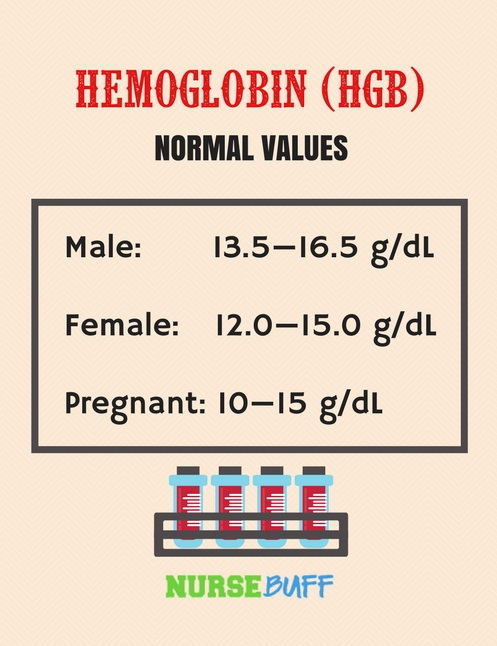
Hemoglobin is the protein component of red blood cells. It makes the blood look bright red as it is made with iron.
High hemoglobin levels are usually present among people living in high altitude levels and among smokers. It’s the body’s way of compensating to a low supply of oxygen.
On the other hand, low hemoglobin levels may be present in a variety of blood diseases, like sickle cell disease and thalassemia.
Normal range:
Male: 13.5—16.5 g/dL
Female: 12.0—15.0 g/dL
Pregnant: 10—15 g/dL
High Level: Dehydration, cigarette smoking, polycythemia vera, tumors, erythropoietin abuse, lung diseases, blood doping.
Low Level: Nutritional deficiencies, blood loss, renal problems, sickle cell anemia, bone marrow suppression, leukemia, lead poisoning, Hodgkin’s lymphoma.
Drugs that may increase hemoglobin: Erythropoietin, iron supplements.
Drugs that may decrease hemoglobin: Aspirin, antibiotics, sulfonamides, trimethadione, anti-neoplastic drugs, indomethacin, doxapram, rifampin, and primaquine.
C. Hematocrit (Hct)
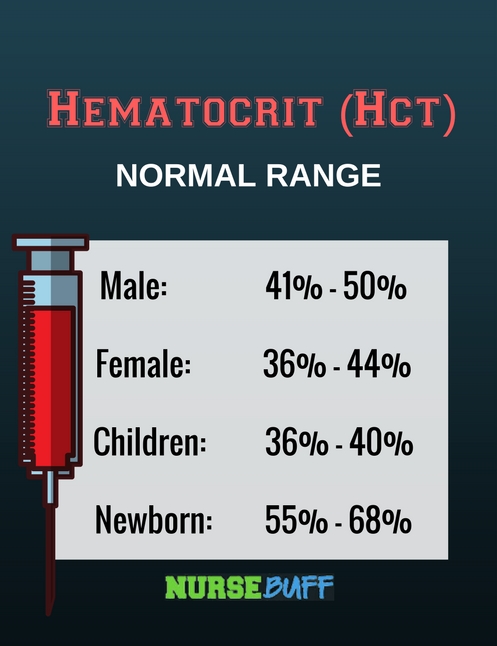
Hematocrit is also known as packed cell volume or PCV. It reflects the volume percentage of red blood cells in the whole blood. The result is dependent on the size, structure, and total number of red blood cells.
Determining hematocrit is helpful in diagnosing and assessing blood diseases, nutritional deficiencies, and hydration status.
Normal range:
Male: 41% – 50%
Female: 36% – 44%
Children: 36% – 40%
Newborn: 55% – 68%
High Level: Dehydration, hypoxia, cigarette smoking, polycythemia vera, tumors, erythropoietin abuse, lung diseases, blood doping, erythrocytosis, cor pulmonale
Low Level: Overhydration, nutritional deficiencies, blood loss, bone marrow suppression, leukemia, lead poisoning, Hodgkin’s lymphoma, chemotherapy treatment
Drugs that may increase hemoglobin: Erythropoietin, iron supplements
Drugs that may decrease hemoglobin: Aspirin, antibiotics, anti-neoplastic drugs
D. Platelet Count
Platelets are also known as thrombocytes. They circulate in the bloodstream and bind together to form a clot over any damaged blood vessel. Determining platelet count is vital in assessing patients for tendencies of bleeding and thrombosis.
Normal range:
150,000 to 400,000 per microliter
High Level: Cancer, allergic reactions, polycythemia vera, recent spleen removal, chronic myelogenous leukemia, inflammation, secondary thombocytosis
Low Level: Viral infection, aplastic anemia, leukemia, alcoholism, vitamin B12 and folic acid deficiency, systemic lupus erythematosus, hemolytic uremic condition, HELLP syndrome, disseminated intravascular coagulopathy, vasculitis, sepsis, splenic sequestration, cirrhosis
Drugs that may increase platelet: Romiplostim, steroids, human IgG, immunosuppressants
Drugs that may decrease platelet: Aspirin, hydroxyurea, anagrelide, chemotherapeutic drugs, statins, ranitidine, quinidine, tetracycline, vancomycin, valproic acid, sulfonamides, phenytoin, piperacillin, penicillin, pentoxifylline, omeprazole, nitroglycerin
E. White Blood Cell
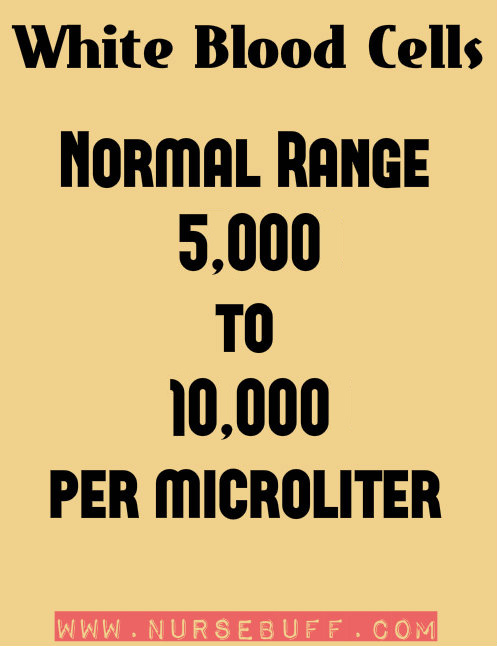
White blood cells, also known as leukocytes, defend the body against infections and other foreign bodies. In general, there are five types of white blood cells– neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
Normal range:
5,000 – 10,000 per microliter (Some textbooks say 4,500 – 10,000)
High Level: Infections, cigarette smoking, leukemia, inflammatory diseases, tissue damage, severe physical or mental stress
Low Level: Autoimmune disorders, bone marrow deficiencies, viral diseases, liver problems, spleen problems, severe bacterial infections, radiation therapy
Drugs that may increase white blood cells: Corticosteroids, heparin, beta-adrenergic agonists, epinephrine, granulocyte colony-stimulating factor, lithium
Drugs that may decrease white blood cells: Diuretics, chemotherapeutic drugs, histamine-2 blockers, captopril, anticonvulsants, antibiotics, antithyroid drugs, quinidine, chlorpromazine, terbinafine, clozapine, sulfonamides, ticlopidine
![]()
II. Urinalysis
![]()
Urinalysis is usually done as part of routine diagnostic examinations. It’s a supportive tool for diagnosing illnesses. A standard urinalysis involves three stages– visual exam, dipstick test and microscopic exam.
A. Visual Examination
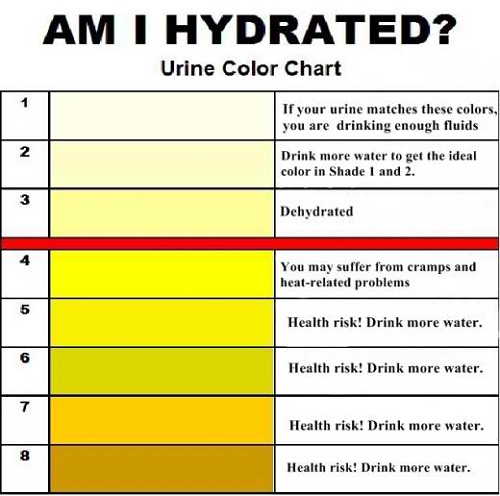
In a visual examination, a urine sample is inspected for color, cloudiness, and odor. It’s supposed to be clear but certain medications and food can affect its color. The presence of bacteria can also affect its appearance:
Here are some examples:
- Clear to dark yellow – normal
- Amber to honey yellow – dehydration
- Orange – dehydration, intake of rifampicin, consumption of orange food dye
- Brown ale – severe dehydration, liver disease
- Pink to reddish – consumption of beets, rhubarb or blueberries, mercury poisoning, tumors, kidney diseases, prostate problems, UTI
- Blue or green – consumption of asparagus, genetic disorders, excess calcium, heartburn medications, multivitamins
- Deep purple – porphyria
B. Dipstick Urine Test
The dipstick urine test is done by dipping a plastic strip into the urine sample. This strip has partitions impregnated by different chemicals that correspond to certain substances present in the urine, so abnormalities will be detected.
Once the strip is dipped into the urine, there will be some changes in the color of the partitions. The following are the chemical tests usually included in reagent strips:
- pH
The pH level of the urine is related to the acid-base balance maintained by the body. Therefore, consumption of acidic or basic foods, as well as the occurrence of any condition in the body that produces acids or bases, will directly affect the pH of the urine. In some circumstances, too acidic or basic urine produces crystals. When this phenomenon happens inside the kidney, kidney stones can develop.
- Specific Gravity
Specific gravity reflects how concentrated the urine is. It can measure the proportion of solutes present in the urine when compared to pure water. Determining specific gravity is useful when you want to detect a particular substance in the urine sample.
For example, if you suspect that a patient secretes small amounts of protein in the urine, the first morning-void urine is the best sample because it has high specific gravity and appears concentrated.
- Protein
Albumin is usually the first type of protein compound excreted in the urine whenever there is a kidney problem. Other types of protein compounds are not detectable in dipstick test and can be measured through a different urine protein test. Conditions that usually produce high amounts of protein in the urine include preeclampsia, multiple myeloma, inflammation, urinary tract injuries, malignancies and other disorders that destroy red blood cells.
- Glucose
Glucose should not be present in the urine. However, in some circumstances, the renal threshold allows the excretion of glucose in the urine when the blood glucose levels are too high. The conditions that can cause glucosuria are pregnancy, diabetes mellitus, liver diseases and hormonal disorders.
- Ketones
Like glucose, ketones should not be present in the urine. Ketones are by-products of fat metabolism and they form whenever there is not enough carbohydrate present for energy production. Ketones also form when insulin levels are not enough to initiate carbohydrate metabolism so the body just uses fat in order to produce the energy needed for daily activities.
Other conditions that produce ketones in the urine are diabetes mellitus, frequent vomiting, strenuous exercise, and high protein diet.
- Blood
The presence of blood in the urine is called hematuria and this usually happens when there is an injury in the urinary tract. Other conditions that may induce hematuria include cigarette smoking, strenuous exercise, kidney problems, and trauma.
- Leukocyte Esterase
Leukocyte esterase is the enzyme produced by white blood cells. Normally, there are white blood cells present in the urine, but they are so few that there is no leukocyte esterase detectable in dipstick test.
On the other hand, when there are many white blood cells present in the urine, the leukocyte esterase level elevates and it could be detected in strips. White blood cells in the urine increase in response to urinary tract infections.
- Bilirubin
Bilirubin, a part of bile, is the yellow fluid secreted into the intestines to aid in digestion. It’s considered a waste product produced by the liver.
It should not be present in a normal urine sample but once detected, it can reflect the presence of liver diseases.
- Urobilinogen
Urobilinogen is formed from bilirubin. It is excreted in the urine in small amounts.
High urobilinogen levels in the urine can signify liver diseases and other conditions that can cause RBC destruction. For people with liver problems and obvious signs of liver dysfunction, the absence of urobilinogen may indicate the presence of a hepatic or biliary obstruction.
- Nitrite
When a bacterial infection is present in the urinary tract, the bacterial flora converts the urine’s nitrate compound to nitrite. However, the detection of nitrite in the urine is not used as a sole basis for the determination of UTI as some people can still have UTI with a negative nitrite result.
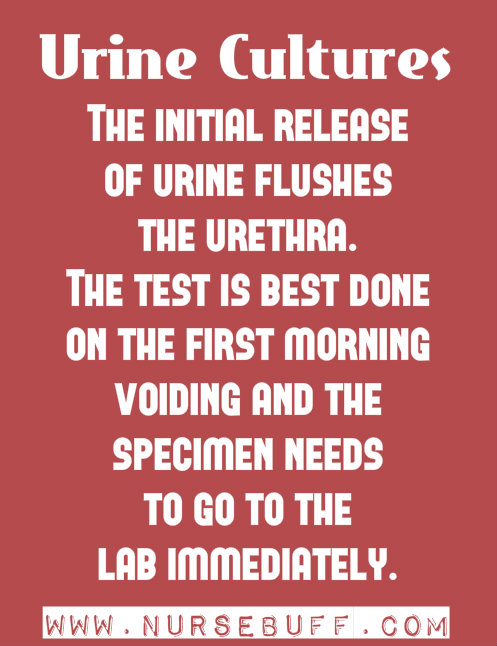
C. Microscopic Examination
In microscopic examination, the urine sample is centrifuged so sediments will settle at the bottom and the clear part can be discarded. Few drops of this centrifuged urine will be examined under a microscope. The sediments observed under the microscope are measured in terms of per lower power field (LPF) or per high power field (HPF).
Some other entities are also measured by estimations like “few”, “many” or “moderate”. The following are the entities measured in a microscopic examination:
- Red blood cells (RBCs)
RBCs are present in the urine sample of a person with severe urinary tract infection, renal disorders, urinary tract injuries and inflammation. It can also reflect an improper collection of urine specimen (e.g. Urine contaminated by blood from menstruation or hemorrhoids).
- White blood cells (WBCs)
Elevated WBCs in the urine is a sign of an infection or inflammation of the urinary tract. It can also reflect improper urine sample collection as in the case of urine specimen contaminated by vaginal secretions.
- Epithelial cells
In a normal urine specimen, there are few epithelial cells that can be seen under microscopic examination. However, in cases of severe urinary tract infection, inflammation and malignancies, there will be an increased number of epithelial cells in the urine.
An elevated number of epithelial cells can also signify an improper collection of the urine specimen, especially if it is not collected using the midstream-catch technique.
- Microorganisms
A normal urine sample is ideally sterile and free from microorganisms. However, in cases of urinary tract infection and improper urine collection, bacteria, yeast, and trichomonads can be found under microscopic examination. Results should be correlated clinically as these microorganisms are also present externally in the genitals.
- Casts
Casts are cylindrically shaped particles formed from the coagulated protein secreted by renal cells. In normal circumstances, these casts are clear and called “hyaline” casts.
When there are kidney problems present, the casts have different components inside, like RBCs or WBCs. Examples include fatty casts, granular cast, and waxy casts among others.
- Crystals
Crystals can be formed from the solutes of urine, especially if it’s concentrated or when its pH is too high or too low. Examples of casts that are not typically present in the urine include leucine, cystine, and tyrosine. These casts may signify malignancies and abnormal metabolic processes.
![]()
III. Serum Electrolytes
![]()
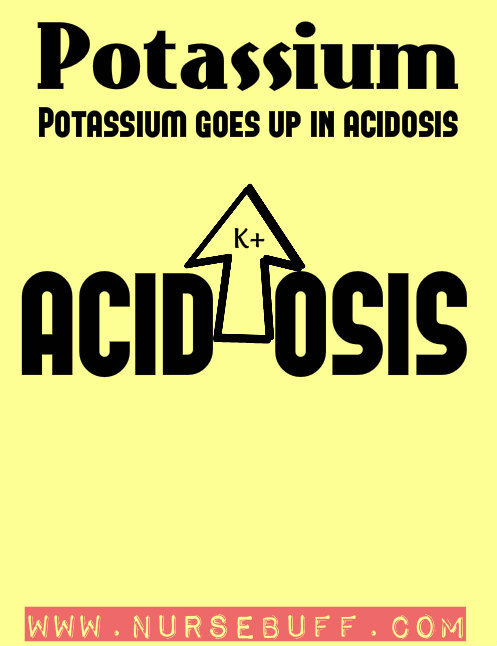
A. Potassium
Potassium is critical in nerve and muscle function because it communicates impulses. The movement of nutrients into the cell and the transport of waste products out of the cell are also mediated by potassium.
Whenever potassium levels are increased or decreased, the heart rhythms are affected as signified by EKG changes.
Normal range:
3.5 – 5.5 milliequivalents per liter (mEq/L)
High Level: Infection, dehydration, Addison’s disease, injury to tissue, diabetes, acute or chronic kidney failure, hypoaldosteronism
Low Level: Anorexia nervosa, malnutrition, diarrhea, vomiting, poorly managed diabetes, hyperaldosteronism
Drugs that may increase potassium: ACE inhibitors, beta blockers, NSAIDs, potassium-sparing diuretics
Drugs that may decrease potassium: Amphotericin B, gentamicin, carbenicillin, corticosteroids, beta-adrenergic agonists, potassium-wasting diuretics
B. Sodium
Sodium reflects a part of renal function as kidneys are responsible for eliminating it from the body. It also plays a part in motor and nerve function.
Patients are tested for serum sodium levels in cases of dehydration, edema, abnormal blood pressure levels, and changes in motor functions.
Normal range:
135 to 145 milliequivalents per liter (mEq/L)
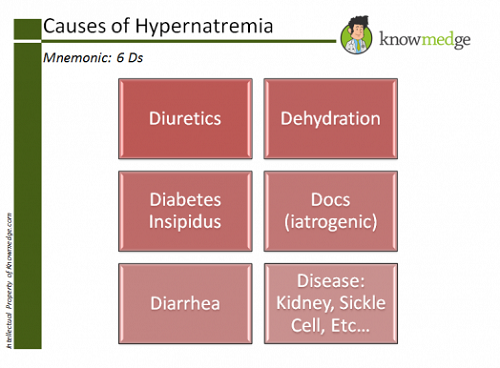
High Level: Cushing syndrome, diabetes insipidus, excessive fluid loss, malnutrition, dehydration
Low Level: Addison’s disease, renal diseases, cirrhosis, heart failure, ketonuria
Drugs that may increase sodium: NSAIDs, laxatives, birth control pills, corticosteroids, and lithium
Drugs that may decrease sodium: Diuretics, morphine, and SSRI antidepressants
C. Chloride
Together with sodium, potassium and carbon dioxide, chloride maintains the normal acid-base balance of the body through balancing body fluids. Abnormal changes in serum chloride levels is usually an indicator of metabolic changes in the body.
Normal range:
95 – 105 milliequivalents per liter (mEq/L)
High Level: Diarrhea, metabolic acidosis, compensated respiratory alkalosis, renal tubular acidosis, bromide poisoning, kidney diseases, Cushing syndrome, hyperventilation
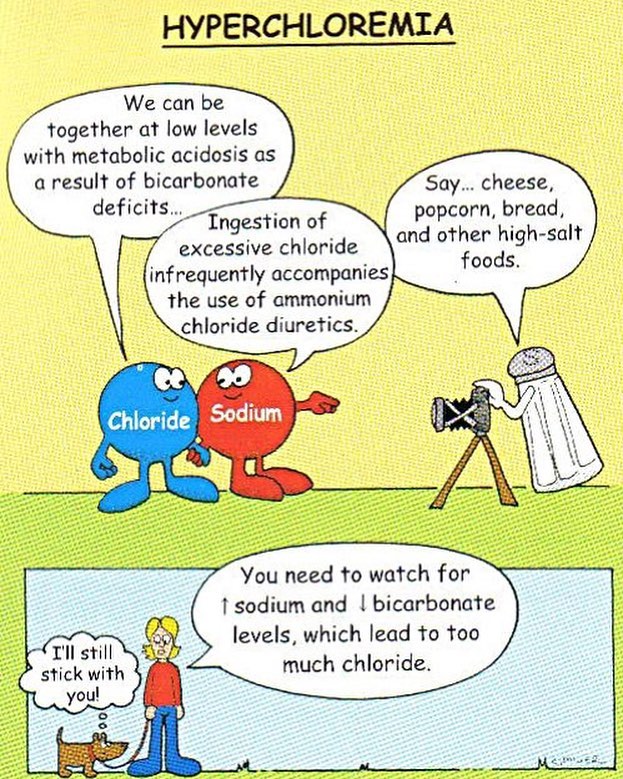
Low Level: Vomiting, burns, excessive sweating, dehydration, gastric suction, chronic lung diseases, Addison’s disease, Bartter syndrome, congestive heart failure, metabolic alkalosis, compensated respiratory acidosis, hyperaldosteronism, syndrome of inappropriate diuretic hormone secretion (SIADH)
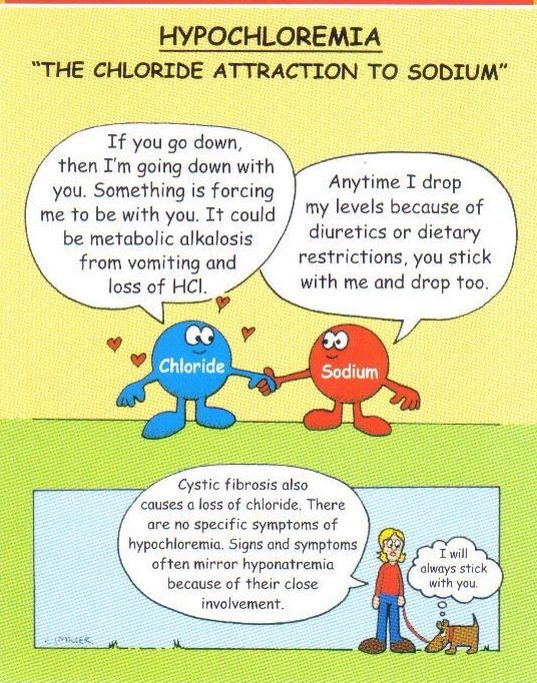
Drugs that may increase chloride: Carbonic anhydrase inhibitors
Drugs that may decrease chloride: Diuretics
Also Read: Nursing Mnemonics and Acronyms (Acid-Base, Fluids, and Electrolytes)
D. Calcium
Calcium is usually binded with protein in the blood. For this reason, a standard calcium test can be misleading and determination of ionized calcium is recommended. The ionized calcium test measures the calcium that is not attached to proteins.
Determining serum calcium levels is important if the patient is suffering from existing nerve and motor dysfunctions.
Normal range:
8.5 to 10.9 mEq/L
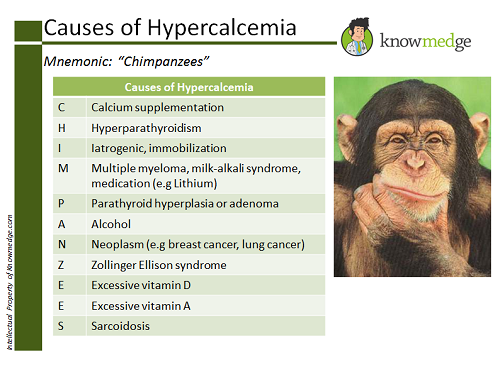
High Level: Tuberculosis, fungal and mycobacterial infections, HIV/AIDS, hyperparathyroidism, metastatic bone tumor, Paget’s disease, multiple myeloma, osteomalacia, sarcoidosis, hyperthyroidism
Low Level: Malnutrition, vitamin D deficiency, hypoparathyroidism, low blood level of albumin, kidney failure, magnesium deficiency, liver disease, osteomalacia, pancreatitis
Drugs that may increase calcium: Lithium, tamoxifen, thiazides, calcium supplements, vitamin D supplements
Drugs that may decrease calcium: No known drug
E. Magnesium
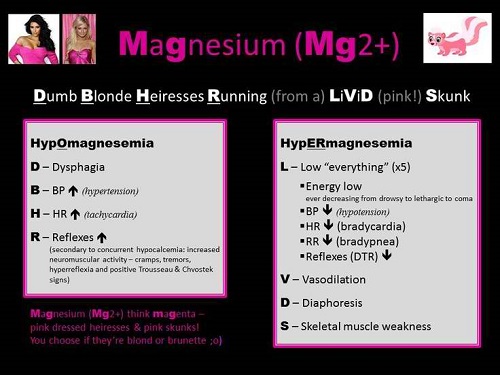
Magnesium is important in muscle and nerve functions, blood pressure regulation, and immune system. It also plays a role in blood sugar regulation.
Although half of the magnesium in the body is stored in bones, magnesium can also be found in cells of organs and body tissues. Its level is checked and tested whenever there are changes in motor functions or when patients are suspected of metabolic diseases.
Normal range:
1.5 to 2.5 mEq/L
High Level: Oliguria, dehydration, Addison disease, chronic renal failure, diabetic acidosis
Low Level: Chronic diarrhea, alcoholism, hemodialysis, ulcerative colitis, delirium tremens, hypoparathyroidism, hyperaldosteronism, hepatic cirrhosis, pancreatitis, toxemia of pregnancy
Drugs that may increase magnesium: Milk of magnesia, lithium carbonate
Drugs that may decrease magnesium: Insulin, antiarrhythmic drugs, digoxin amiodarone, sotalol, quinidine, bretylium, strophanthin, diuretics, isoproterenol
F. Phosphorus
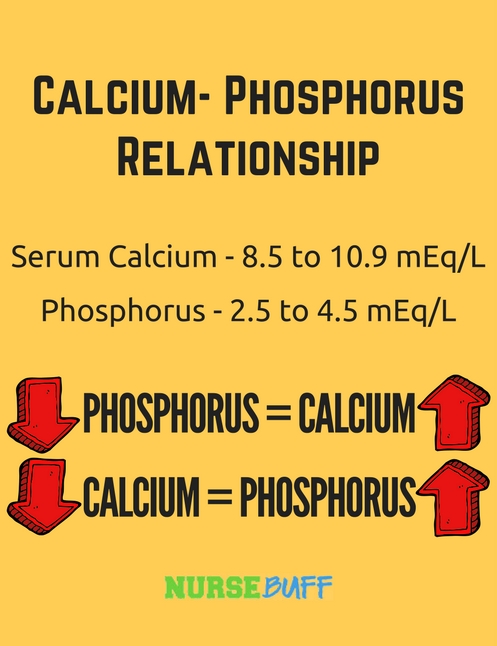
Phosphorus is involved in the intracellular metabolism of proteins, fats, and carbohydrates. It also participates in the production of ATP. It’s the chemical compound that supplies energy to the cell.
Phosphorus plays an important role in the acid-base balance of the body and in glycolysis.
Normal range:
2.5 to 4.5 mEq/L
High Level: Hypoparathyroidism, diabetic ketoacidosis, liver disease, kidney failure
Low Level: Poor nutrition, alcoholism, hyperparathyroidism, hypercalcemia
Drugs that may increase phosphorous: Vitamin D, phosphate-containing laxatives
Drugs that may decrease phosphorous: Antacids, diuretics, corticosteroids, anticonvulsants, ACE inhibitors, insulin
![]()
IV. Renal Function Tests
![]()
A. Blood Urea Nitrogen (BUN)
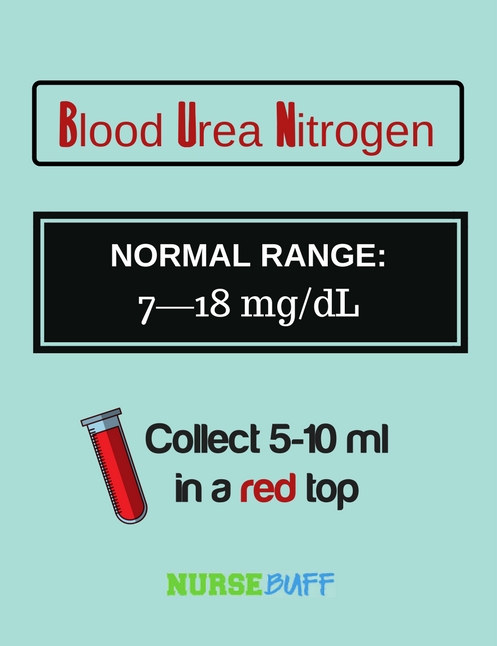
BUN is a by-product of protein metabolism. This test is used to determine the adequacy of renal function but it may also produce a false-positive result as it is dependent on renal blood flow, protein metabolism, catabolism, drugs, and diet.
BUN can also reflect protein tolerance, hydration status, degree of catabolism, and risk of uremic syndrome.
Normal range:
7—18 mg/dL
High Level: Hypovolemia, excessive protein levels in the gastrointestinal tract, congestive heart failure, gastrointestinal bleeding, heart attack, urinary tract obstruction, glomerulonephritis, pyelonephritis, acute tubular necrosis, kidney failure, shock.
Low Level: Low protein diet, malnutrition, liver failure, fluid overload.
Drugs that may increase BUN: Allopurinol, furosemide, indomethacin, cisplatin, methyldopa, propanolol, tetracyclines, rifampin, vancomycin, thiazide diuretics, gentamycin, carbamazepine, aminoglycosides, amphotericin B.
Drugs that may decrease BUN: Streptomycin, chloramphenicol.
B. Creatinine
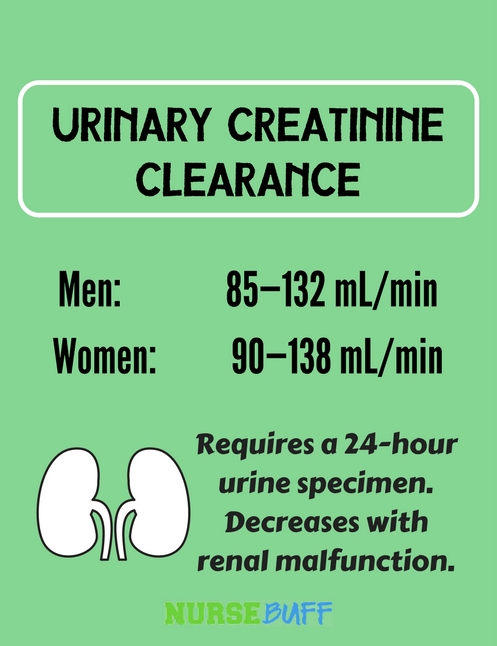
Creatinine is the product of muscle metabolism. Whenever there is an elevation in serum creatinine levels, renal dysfunction is usually suspected since the kidneys are responsible for the excretion of creatinine in the body.
In general, creatinine levels vary depending on a person’s body size and muscle mass.
Normal range:
Men: 85—132 mL/min
Women: 90—138 mL/min
High Level: Preeclampsia, dehydration, renal problems, rhabdomyolysis, blocked urinary tract, myasthenia gravis, hyperthyroidism, muscular dystrophy
Low Level: Spinal cord injuries, cachexia, sudden decrease in activity
Drugs that may increase creatinine: Aminoglycosides, methicillin, amphotericin B, cistplatin, dextran, cyclosporine, gallium, lithium, hydroxyurea, methoxyflurane, nitrofurantoin, plicamycin, pentamidine, streptozocin
Drugs that may decrease creatinine: Neuromuscular blocking agents